As we walk through life, our losses walk with us. How do we begin the process of making peace with the concepts of death and grief? What happens to those of us who are left behind? How can we learn to live again? This podcast examines these questions and more. It was recorded in front of a live audience for the Conference on World Affairs at the University of Boulder.
2014 May

Two quick reminders today and then you can go back to the awesomeness I hope your day is bringing.
First – Remember to send in your designs for my new “I Am Enough” t-shirt. Currently, you’ve sent in 7 great designs and this one is in the lead!
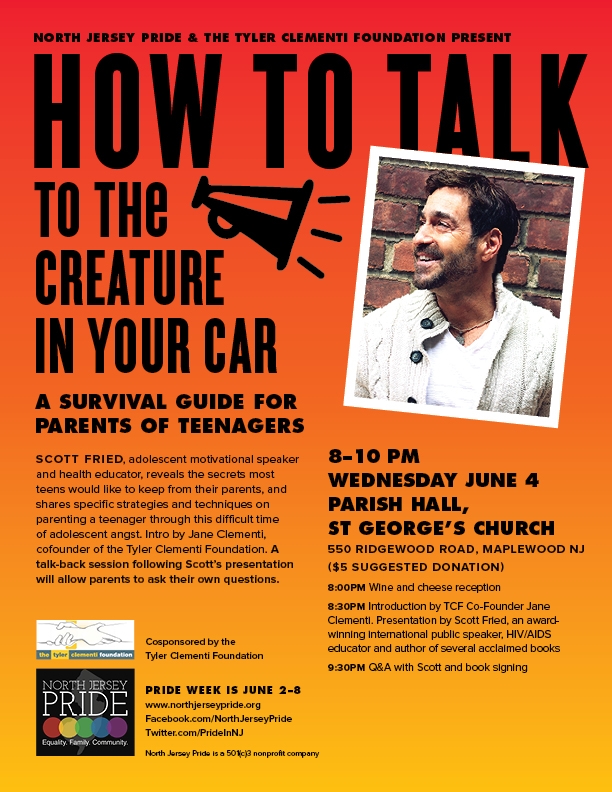
Second – for you parents and caring others in New York and New Jersey, I’ll be teaching at an event hosted by the Tyler Clementi Foundation and North Jersey Pride. Both the Facebook event or the flyer have all the information. It’s such an honor to work with Jane Clementi and the Tyler Clementi Foundation and I hope to see you there.

Name:
sarah
Age:
14
Who Are You?
i don’t know, but then again, who does?
Whose arms do you fall into?
my best friend’s: she is the world to me. Maybe one day there will be a guys arms i can fall into.
What is the one miracle you are waiting for?
i guess i don’t really know
What is your weapon?
i flirt when i want something, but one time i took it too far. i got a hurt. more than just a little bit hurt. be careful about what u do and how far u take it, lets just say i ran to the wrong base.
Whom do you miss the most?
my friend who died last year. i miss him.
What are you scared of?
getting hurt again. i dont want to be used again. my body is mine and no one else’s.
What is your favorite memory?
When i was overlooking a waterfall with my best friend.
When was the last time God spoke to you and what did He say?
i don’t know….
What words are you holding onto in your pockets?
I’m scared. i try to make people believe that I’m stronger than i really am.
What’s the best advice you’ve ever been given?
stay true to yourself.
What advice would you give to your parents that will help them in raising you?
Don’t judge, everyone makes mistakes.
Is there sometimes an emptiness inside you and what does it feel like?
yes. my friend is gone. i just want him back on this earth.
Are you enough?
i am enough. everyone is enough. i think that’s something that people need to learn. you are enough.

HPV stands for human papillomavirus, which is a virus from the papillomavirus family that affects human skin and the moist membranes that line the body, such as the throat, mouth, feet, fingers, nails, anus and cervix. There are at least 120 types of HPV. Some of them cause the kind of common warts you see on people’s hands and some of them cause plantar warts on the feet.
About 40 types of HPV, however, can infect the genital area — the vulva, vagina, cervix, rectum, anus, penis, or scrotum.
Genital HPV infections are very common. HPV is so common that about half of all men and more than 3 out of 4 women have HPV at some point in their lives. But most people who have HPV don’t know it.
For the purposes of understanding HPV better, let’s group it into two categories: low risk and high risk.
Here’s how it works: the papilloma viruses infect cells just beneath the skin which, like normal skin cells, move toward the surface, reach the upper layer, die and slough off, quite unnoticed by anyone. Papilloma is a fancy word for “raised bump,” so occasionally, the HPV-infected cells form lumps, which can be seen and felt. In reality, these are benign tumors. They are more commonly called genital warts.
Genital warts are warts that are located near or on the genital areas. In a female, that means on or near the vulva (the outside genital area), vagina, cervix, or anus. In a male, that means near or on the penis, scrotum, or anus.
Genital warts can look like bumps or growths. They can be flat or raised, single or many, small or large. They tend to be whitish or flesh colored. Sometimes, if left untreated, they can be shaped like a cauliflower. They are not always easy to see with the naked eye, and many times a person with genital warts doesn’t know that they’re there.
The warts can show up weeks or months after exposure to an infected sexual partner.
The types of HPV that can cause genital warts are NOT the same as the types of HPV that can cause cancer. Low-risk HPV strains, such as HPV-6 and 11, cause more than 90% of genital warts, which rarely develop into cancer. These, along with HPV-42, 43 and 44 are LOW risk for cancer of the cervix.
In the majority of cases, infected young females are not infected for long and there is no long-term consequence. The CDC says that over 70% of young female infections clear up within 12 months, while 90% do so within 24 months.
Not all of the 40 sexually transmitted HPV viruses cause serious health problems. But there are some types of HPV that may cause cell changes, which sometimes lead to cervical cancer and certain other genital and throat cancers. These are called high-risk types.
Very few warts are of the high-risk type. High-risk HPV strains include HPV-16 and 18, which cause about 70% of cervical cancers. Other high-risk HPV strains include 31, 33, 35, 39, 45, 51, 52, 58, and a few others.
Although most HPV infections go away within 8 to 13 months, some will not. HPV infections that do not go away can “hide” in the body for years and not be detected. That’s why it is impossible to know exactly when someone got infected, how long they’ve been infected, or who passed the infection to them.
In somewhere between 5% to 10% of cases, the infection persists and leads to high-risk type of HPV. This persistent long-term HPV infection raises the risk of developing precancerous lesions of the cervix. These can eventually, over a period of five to ten years, develop into cervical cancer. During this period, the progress can be treated and reversed with treatment for the pre-cancerous lesions. In some cases, treatment can lead to loss of fertility. However, in the majority of cases, cancer can be prevented.
As mentioned earlier, in 90% of cases the body’s own immune system destroys all the HPVs within 24 months. It is impossible to tell who might go on to develop health problems, including cancer.
These sexually transmitted HPV viruses are spread through contact with infected genital skin, mucous membranes, or bodily fluids, and can be passed through vaginal intercourse, anal intercourse and oral sex.
HPV can infect skin not normally covered by a condom, so using a condom does not fully protect someone from the virus.
You can get it from touching (hand to genital or genital to genital) an infected person’s lesions, which can transmit cells containing the virus.
Here’s an interesting fact regarding transmission of HPV: for many people, HPV is transmitted during their first 2 to 3 years of sexual contact.
Experts believe that when a wart is present, the virus may be more contagious. But HPV can still spread even if you can’t see warts. Many people don’t realize they’re infected with HPV and may have no symptoms, so neither sexual partner may realize that the virus is being spread.
In some rare cases, genital warts are transmitted from a mother to her baby during childbirth.
Warts can appear any time from several weeks to several months after a person has been exposed to them. Sometimes they might take even longer to appear because the virus can live in the body for a very long time before showing up as warts.
A few weeks or many months after infection, small groups of the genital warts, the size of a pinhead to begin with, appear on their own or in groups. They grow mostly on the head of the penis or anus. Occasionally, they appear in mouth, on the tongue or other parts of body or face, including the urethra and peri-anal area. Untreated, they can spread and get bigger to cauliflower-like warts.
External lesions may itch. A lesion on the skin may be either papillary (standing up from the skin) or flat. Lesions on the cervix can be seen only with the use of 5% acetic acid and magnification.
Not all warts look the same. They can be flat or raised above the surrounding skin. In moist areas, they have a softer surface and are known as exophytic warts. On skin that’s exposed to the air, the wart has a harder, “keratinized” surface. These are known as sessile or popular warts. Warts can be as small as a pinhead or as large as a sprout.
About 20 million people in the U.S. are infected with HPV at any time, according to the CDC. And three-fourths of sexually active people between ages 15 and 49 have been infected at some point in their lives, according to estimates from the American Social Health Association.
You’re more likely to get HPV if you:
- Have sex at an early age
- Have many sex partners
- Have a sex partner who has had multiple partners
While many people think HPV is mostly a problem for teens or young adults, HPV can infect men and women of any age. In fact, the latest statistics from the CDC found that:
- 19% of women 50 to 59 were infected with HPV virus
- 27% of women 20 to 24 were infected with HPV virus
- 45% of women 14 to 19 were infected with HPV virus
This has already been stated, but it’s important to read it again. Most HPV infections have no signs or symptoms. So someone can be infected and pass the disease on to another person without knowing.
Some people do get visible warts. Although warts might hurt, itch, or feel uncomfortable, most of the time they don’t. This is one reason why people may not know they have them.
Doctors can diagnose warts by examining the skin closely (sometimes with a magnifying glass) and using a special solution to make them easier to see.
Your doctor may take a tissue sample, (biopsy) and then examine it under the microscope (histology).
A common way to diagnose HPV in females is with a Pap smear (routine cervical cytology). This is a test that is performed during a gynecologic exam. In college-age females, probably no more than 10% of cervical lesions are truly pre-cancerous. It is extremely unlikely in college age women that HPV turns out to be malignant.
A colposcopy enables the operator to examine the surface of the cervix under magnification. Biopsies can be taken and if the labs show suspicious cells, it’s a simple matter to remove the offending tissue by freezing, burning or cutting off or a combination of these.
So here’s the thing about HPV: you can treat the symptoms but rarely get rid of the virus. The good news is that the lesions and warts can be eliminated. For many people, the virus is cleared from the body by itself! For others, viral particles remain in a latent form after treatment. However, (more good news), it is doubtful that simple presence of latent viral particles can result in transmission.
It is not possible to predict how long treatment will be needed. In some, two or three ‘shots’ of cryo-therapy suffices, while in others the warts just go on and on. Approximately 25% of cases return within 3 months.
However, in this particular lottery, everyone is a winner. Warts always eventually go away!
Here’s some really technical stuff about HPV treatment. Your doctor might use one or more of these procedures to remove the warts:
- LEEP (loop electrosurgical excision procedure): uses a metal prong, which literally burns the wart away.
- Freezing (cryotherapy) with liquid nitrogen: most commonly used. A jet of liquid nitrogen freezes the wart until it turns white. This is repeated at weekly intervals until the warts are gone. Freezing destroys the skin cell in which the virus resides. The cell dies; the virus dies. There are two theories to freezing warts: one freezes the wart and a small area around it, whereas the other limits the white frozen area to the wart.
- Aldara is a topical cream which is very effective.
- Laser is useful when there are many warts.
- Liquid N, TCA/BCA (tri and bichloracetic acid), and interferon: burns away the wart.
- Podophyllin: a plant extract, stops cells dividing, which means that the virus dies out. It has been replaced by podophyllotoxin. This is the first home treatment. It’s easy for the patient to apply as a cream or lotion – three times weekly, for 4 weeks.
- Imiquimod: an immune modulator is applied 3x a week, for 4 weeks (can be up to 16 weeks).
- 5-flouorocytosine is useful for warts that are difficult to reach, for example inside the urethra in the male.
- Proctoscopy: passing a metal cylinder through the anus to get at the warts. Not highly effective.
Yes, high-risk types of genital HPV can cause cancer of the cervix, vagina, vulva, anus, penis, and throat. The type of cancer HPV causes most often is cervical cancer.
Up to 50% of sexually active women develop HPV on their cervix. But as already stated, infection persists in up to only 10%. Perhaps 1 in five of those will need further treatment to prevent development of cancer.
Most HPV infections go away by themselves and don’t cause cancer. But abnormal cells can develop when high-risk types of HPV don’t go away. If these abnormal cells are not detected and treated, they can lead to cancer.
Most of us recover from HPV infections with no health problems at all. It is not fully known why some people develop long-term HPV infection, precancerous abnormal cell changes, or cancer. But we do know that women who have diseases that make it difficult for them to fight infections are at higher risk of cervical cancer. We also know that cigarette smoking increases the risk of cervical cancer.
There are two vaccines that have been shown to stop infection.
Although the vaccines were primarily designed to reduce the risk of cervical cancer in women, they also reduce the likelihood of genital warts in general and have some effect even on those already infected.
<b>Gardasil</b> protects against HPV type-16 and 18, and as we learned earlier, those are the high-risk strains, which cause 70% of cases of cervical cancer. It also protects against HPV types-6 and 11, the low-risk strains, which cause 90% of cases of genital warts.
<b>Cervarix</b> is another type of HPV vaccine that protects only against HPV types-16 and 18, the high-risk strains.
A patient’s prior exposure to HPV and age are two very important things to consider before s/he receives three doses of the vaccine. Unfortunately, Gardasil does not cure HPV. Gardasil does not work for a person who has already been exposed to the strains of the virus in the vaccine. As far as age goes, the vaccine is recommended for women and men between the ages of 9 and 26. Vaccinating a person before his or her first sexual encounter is thought to be most effective, although the vaccine can also be administered to someone who is sexually active.
If you choose to get the Gardasil vaccine, it is recommended that you have someone with you as you leave. It has been found that some people faint 20 minutes after the shot.
There are at least 120 types of HPVs. Below is a list of HPV virus types and what signs and symptoms or diseases they are linked to:
- 2, 7 – Common warts. Rough, raised bumps that generally affect the fingers, hands and around the nails. In the majority of cases their only problem is their appearance; however, they may sometimes bleed. Some patients may experience pain, but this is unusual.
- 1, 2, 4, 63 – Plantar warts. Small lesions that appear on the soles of the feet; they usually look like a cauliflower, with very small hemorrhages (petechiae) under the skin. When scratched they may bleed. Patients may feel pain when walking or standing. They can be similar to corns or calluses.
- 3, 10, 8 – Flat warts. Slightly raised, flat-topped lesions, which are darker than the skin around them. They may appear on the knees, elbows, wrists, hands, neck or face. Young adults, teenagers and younger children are usually affected.
- 6, 11, 42, 44 and some others – Anogenital warts. Small, flat cauliflower-like bumps, some may have stem-like protrusions. In females, the warts will usually appear on the vulva, but may also be found in the vagina, on the cervix, and near the anus. In males, they may appear on the penis, around the anus, and on the scrotum. They are rarely painful and do not typically cause discomfort.
- 6, 16, 18, 31, 53, 58 – Anal lesions
- Genital cancers - 16, 18, 31, 45 are the highest risk - 33, 35, 39, 51, 52, 56, 58, 59 are high or medium-risk - 26, 53, 66, 68, 73, 82 – are probably high-risk
- 6, 7, 11, 16, 32 – Oral papillomas
- 16 – Oropharyngeal cancer
- 6,11 – Laryngeal papillomatosis
All sorts of lumps or bumps in the genital area get mistaken for warts and there are six other diagnoses that regularly cause confusion.Sebaceous cysts are pockets of secretion from sebaceous glands in the skin and occur almost anywhere. They vary in size from a small ballbearing to a billiard ball or larger.Folliculitis is literally an inflammation of a hair follicle. Any bit of skin that has hair follicles can develop folliculitis, which when infected becomes a boil.Skin tags are little extra bits of skin near the entrance to the vagina or around the anus.Molluscum contagiosum is sometimes mistaken for HPV.
Fordyce tubercles or ‘pearly papules’ appear as a ring of small, whitish bumps less than a millimeter across, encircling the glans penis just where it joins the shaft. They are normal variations but are often misdiagnosed as warts.
Vulval papillosis, a woman’s equivalent to Fordyce tubercles, are little fleshy bumps, also smaller than 1 mm across on the inside of the labia. Both vulval papillosis and Fordyce tubercles will not go away if subjected to anti-wart treatment.Any condition that can cause lumps or bumps on the skin will be confused with warts.
However, the conditions described above will account for 95% of the “warts” that turn out not to be warts.
In pregnancy, the immune system becomes less aggressive so as not to harm the unborn child, allowing warts to surface. Those who know they’ve had warts in the past and those with latent HPV infection may develop warts when they become pregnant. The good news is that the warts tend to regress, even without treatment, after the baby is born.The anogenital HPV types are usually confined to the nether regions. Very rarely, a mother with genital infection can pass this on during birth leading to laryngeal warts in her child.
Because HPV is so common and such a popular topic these days, there are a lot of key points to remember:
- Most HPV infections have no harmful effect at all.
- Most HPV cures itself without any medical intervention.
- There are more than 120 types, half of which cause genital warts.
- Approximately 3 out of 4 people will get them after having any kind of genital contact with someone who is infected.
- While there are 40 types of HPV that affect the genital area, some are low risk and some are high risk that cause most of the HPV-related diseases.
- Low risk strains are types-6 and 11 and cause about 90% of genital wart cases in males and females.
- High risk strains are types-16 and 18 and cause about 75% of cervical cancer cases, 70% of vaginal cancer cases, and up to 50% of vulvar cancer cases in females.
- If you have HPV, you should not be ashamed or afraid. Most people who have had sex have HPV at some point in their lives. And most infections go away on their own.
- The warts are actually (and properly) called ano-genital warts because they favor the back as well as the front. Warts can occur around the anus in both sexes without anal intercourse.
- It is the most common STI in the US.
- More than 5 million people are infected with it each year. 20 million people are currently living with it.
- The highest rates of genital HPV infections are found in adults between the ages of 18 to 28.
- Up to 80% of women will have been infected by the age of 25.
- At least 80% of sexually active women have been infected.
- Less than 5% of women aged 50 or older are still infected.
- HPV may be less common in young men but will infect well over 50%.
- Most of these men and women are unaware and unless they develop actual warts, will go their graves unaffected and oblivious.
- By the age of 50, only a small number, less than 5%, still carry the virus, unless they are still having many sexual partners. This statistic tells us that we eradicate it ourselves eventually.
- You cannot catch genital warts from towels or sheets.
- Keep in mind that a healthy immune system is usually able to clear the HPV virus, or at least suppress it, over time.
- Most men who contract HPV (of any type) never develop any symptoms or health problems.
- Unfortunately, there are no blood tests clinically available to diagnose a person for HPV prior to vaccination. Most of the time, patients are diagnosed when visible genital warts appear.
DISCLAIMER: The information contained in this post is intended to inform readers and is not intended to replace specific advice from a health care professional.

-Vito Russo
It was always interesting sitting next to Phyllis at those meetings. She’d talk out loud and finish people’s sentences under her breath. I suppose for herself and not just for those sitting around her. She grabbed the journal out of my hand and wrote down these words:
“Now that HIV has happened to you, the goal is to learn how to live with a little more gratitude, a little more elegance!”
I wrote down many of my favorite shares from that meeting. Greg, from San Francisco said, “I feel like every cell in my body has a tear to shed.”
Curtis, who had just gotten out of the hospital, shared his experience of lying in bed, preparing to die. “It was just me and God,” he began. “That’s what did it for me. I prayed each night for Him to be with me. Just be with me. And give me peace. And take away all the pain. That’s all.”
Phyllis began to rock back and forth. “That’s all,” she repeated. “That’s all.”
Curtis continued. “It’s just life. We know that. And we all know so many people who have died. So what’s the big deal? I’ll just hang out with them for awhile. ” He paused a moment before he said, “…and, yeah I have fear. I’d lay there with all my fear and think: this is it. So this is it. And then I’d think, what is it? It’s just life.”
Once upon a time, most of my friends died of AIDS. But before they did, they would sit in those support groups and try to find the perfect words to describe their experience.
“I need to make peace with the word ‘AIDS,'” Robert shouted. He was in his angry phase; he had lost his ability to walk. “I want to find a new way to describe my disease. Instead of calling it the Acquired Immuno-deficiency Syndrome, I’m gonna call it ‘Always in Divine Safety.'”
Just then, Ross leaned forward on the white couch. Ross, whose HIV had manifested as a brain tumor, had lost all of his blonde curls from months of chemotherapy and radiation. “I have another one,” he smiled. Ross was always smiling. “I’m gonna call AIDS – ‘Angels in Darth Vader Suits.'”
Curtis and Robert and Ross have died, along with almost everyone in that room that night.
Benji and Phyllis are still alive.
So am I.
It was a time of unexalted destinies. Yet, we still searched for safety and meaning and angels.
This week, if a faithful ache should arrive, think of my friends and try to see the situation as an angel in a Darth Vader suit.
How can you live with a little more gratitude?
How can you live with a little more elegance?
Each of us is at risk of having a broken heart. It takes great courage to believe in love; to believe that love is worth the cost of breathing; the price of the pulse of blood in your veins; the gathering of a million mornings of hope. It is a holy thing to love what can change. It is a courageous thing to love what can leave. This podcast, recorded in front of a live audience, is for guys like me. The song was written by Mary Chapin Carpenter.
Please join me for an important event on Tuesday, June 4th. I’m giving a lecture entitled, “How to Talk to the Creature in Your Car: A Survival Guide for Parents of Teens,” where I’ll be sharing specific strategies and techniques on parenting a teenager through the arc of adolescence.
It’s a presentation that will validate the successful things that are already working in your relationship with your teen. Or, you can use it as a survival guide to communicating with the creature listening to music in your car. Mostly, I hope the evening will be a gentle reminder of what every teen wants more than anything else: the tender presence of a loving other and permission to be whomever they are becoming.
I’ve very excited about this event and want to thank Jane Clementi of The Tyler Clementi Foundation (Tyler’s mom) and North Jersey Pride for making this possible. Tyler’s family will be there and Jane will be giving the introduction.
The full flyer is below and you can register to attend on the Facebook event here.
I hope to see you there!

Name:
Alyson
Age:
23
Who Are You?
I’m gay. I’m both male and female and neither male nor female. I’m everything I’m not supposed to be. Nine times out of ten, I’m the one being bullied, the one putting everything on the line only to have it thrown back in my face.
Whose arms do you fall into?
I haven’t fallen into anyone arms yet. I’m still waiting for a knight(ess) in shining armor to come rescue me from this hell.
What is the one miracle you are waiting for?
To be able to live a day when I’m glad to be alive.
What is your weapon?
Myself. Isolation.
Whom do you miss the most?
EB…may she rest in peace after dying this past year by her own hands.
What are you scared of?
Dying. Living. Sex. Pleasure.
What is your favorite memory?
Telling on myself (to an adult) before I pulled the plug to end my life. Reaching out for help and submitting myself to going to the emergency room to stop myself from acting upon my urges.
When was the last time God spoke to you and what did He say?
She said how I’m beautiful and I deserve to live free of fear.
What words are you holding onto in your pockets?
The wish of “la libertad de nao sentir medo” (The freedom to not be afraid)
What’s the best advice you’ve ever been given?
Someone, somewhere in this world, is waiting to meet you.
What advice would you give to your parents that will help them in raising you?
Don’t ever doubt your child of his/her potential.
Is there sometimes an emptiness inside you and what does it feel like?
Yes. It feels like being locked in my dog’s cage. Or like the time I had to eat dinner after visiting Auschwitz.
Are you enough?
No. I think if I were enough I would not be so dependent on self-loathing jokes.

Who remembers where this quote is from?
“You gave me syphilis?”
Answer: Grey’s Anatomy – Season One, Episode 9. George discovers he has syphilis, and it soon emerges that the disease is rampant among the hospital staff.
Well, just last week, the CDC (U.S. Centers for Disease Control and Prevention) announced that syphilis has returned with a vengeance to the gay community. Once almost eliminated in the United States, cases of syphilis have more than doubled among gay and bisexual men since the year 2000.
If you’re a numbers kind of person, this might interest you. In 2013, there were more than 16,000 cases of syphilis, 91% of these in men – up from 84% in 2012.
So this week’s STI topic is all about syphilis.
Syphilis is caused by a type of bacteria known as a spirochete, called treponema pallidum that lives in warm, moist parts of the body such as the mouth, anus and penis. If you were to look at it through a microscope, you’d see something that looks like a corkscrew or spiral. It’s extremely small and can live almost anywhere in the body.
These spirochetes can be passed from one person to another through direct contact with a syphilis sore (infectious lesion). That contact can be genital intercourse, anal intercourse or oral intercourse. Yes, that means that you can get syphilis from oral sex. The bacteria pass through intact mucous membranes and abraded (just a fancy word for scraped) skin. The treponeme needs a small cut or abrasion in the skin to cause infection which may be one of the reasons it is common among MSM (men having sex with men), since anal intercourse is more traumatic than vaginal sex. The spirochetes are then carried by the bloodstream to every organ in the body. The infection can also be passed from a mother to her baby during pregnancy. But listen up…you cannot catch syphilis from a towel, doorknob, or toilet seat.
In its early stages, syphilis is easily treatable. However, if left untreated, it can cause serious problems — even death. So it’s important to understand as much as you can about this disease.
A person who has been exposed to the spirochetes that cause syphilis may notice a chancre from 10 days to 3 months later, though the average is 3 weeks. If the syphilis is not treated, the second stage of the disease may occur anywhere from about 2 to 10 weeks after the original sore (chancre).
It’s important to keep in mind that many people never notice any symptoms of syphilis. This means it is important to let your doctor know that you are having sex, so that he or she can test you for syphilis even if you don’t have any symptoms.
So this is where it gets interesting. Syphilis is divided into three stages, each with different signs and symptoms.
Primary Stage: Syphilis usually appears first as a red, firm, painless and sometimes wet ulcer or open genital sore, which disappears without a scar. “It can appear in the back of the throat and be missed entirely,” according to Dr. Demetre Daskalakis, an infectious disease expert at Mount Sinai Hospital in New York City. This first phase is the most infectious stage.
This chancre (pronounced: SHANG-ker) appears 3 weeks to 90 days (up to 12 weeks) after infection either on the penis, scrotum, mouth, back of the throat or anus. It’s often misdiagnosed as a herpes sore. It then scabs over and heals. Also, the glands nearest to the sore (neck or groin) may swell. Treatment of the sore with antiseptics or antibiotic creams has no effect since the treponeme has already infected the nearby lymph nodes. The sore is usually painless (as are the swollen nearby lymph glands) and feels like a small hard button just below the skin surface. It varies between barely visible to the size of a small fingernail.
The primary chancre is usually a single ulcer that is hard to miss when found on the penis but difficult when on the vulva, vagina or cervix, or in either gender when near the anus. A chancre can be found on the lips, nipples, tongue or other sites. One unlucky site is the base of the penis (called a “condom chancre”) when a sore on the vulva has come into contact with the lower part of the penis NOT covered by the condom.
The chancre will disappear on its own in 1-6 weeks (3 weeks average) but the disease doesn’t go away. In fact, if the infection hasn’t been treated, the disease will continue to get worse.
The primary sore is still present in perhaps 15% of secondary stage cases.
Secondary Stage: About 3-8 weeks after infection, the bacterium has spread throughout the body. A rash appears in most people on hands, palm and the soles of the feet. It might seem like this rash is the most important problem. But the treponeme can be found affecting all the parts of the body, from the liver to the lungs and the brain to the bones. People with secondary syphilis feel generally unwell, with a temperature, aches and pains, and loss of appetite. Half have enlarged lymph glands. Other symptoms are condylomata lata (fancy term for wart growths), lymph node enlargement, spotty baldness/hair loss, mild fever, fatigue, ulcers in the mouth and anus, and weight loss. There is an involvement of the central nervous system in 20% of cases, with nothing more than a slight headache.
Sometimes the rashes associated with syphilis can be very faint or look like rashes from other infections and, therefore, may not be noticed. Remember, sores sometimes appear on the lips, mouth, throat, vagina, and anus — but many people with secondary syphilis don’t have sores at all.
Secondary symptoms may last 2 to 6 weeks (4 weeks average) and may recur. The symptoms of this secondary stage will go away with or without treatment. But if the infection hasn’t been treated, the disease can continue to progress. Syphilis is still contagious during the secondary stage.
After some weeks, the rash and other complications disappear and the disease enters its next stage.
Early latent stage: If syphilis still hasn’t been treated, the person will have a period of the illness called latent (hidden) syphilis. This means that all the signs of the disease go away, but the disease is still very much there. Even though the disease is “hiding,” the spirochetes are still in the body. This stage can last for 2 years without signs or symptoms although infectious bacteria are still present in the tissues. Syphilis can remain latent for many years. Chancres or rashes may recur in this early latent stage.
Late latent stage or Tertiary Stage: If the disease still hasn’t been treated at this point, some develop tertiary (or late-stage) syphilis. This means the spirochetes have spread all over the body and can affect the brain, the eyes, the heart, the spinal cord, and bones. Symptoms of late syphilis can include difficulty walking, numbness, gradual blindness, and possibly even death. One third of people reach this stage, also called neuro-syphillis. It can appear up to 30 years after infection. The good news is that there is no chance of syphilis being passed on in this stage. It’s also been found that many who have reached this stage can look forward to no further trouble from their infection and may die of old age or an unrelated condition. The lesion in tertiary syphilis is known as the gumma. A gumma results from blockage of small arteries and can cause spots and lumps or nodules in skin, tongue, bones, muscles and internal organs. These later manifestation of syphilis are very uncommon in the western world today. If untreated, there can serious damage to the nervous system, heart, brain and other organs. Sometimes no clinical signs, but vascular and neurological damage may be occurring.
There is something called a dark-ground or dark-field microscope examination that looks at a little fluid from the primary sore of the secondary rash. Also, serological tests measure the presence of antibodies in the blood.
– Treponemal antibody tests, TPHA, TPPA, FTA or EIA stay positive forever even after successful treatment. These continuing positive results simply say that the person has had the infection in the past.
– Non-treponemal antibody tests, VDRL and the RPR tell us whether the syphilis is still active, depending on how strongly positive the test is. This distinguishes between a positive treponemal test owing to older treated infection or a new infection.
If you think you may have syphilis or if you have had sexual contact with someone who might have syphilis, see your doctor or gynecologist right away. It can sometimes be difficult to spot chancres. So it’s important to get checked on a regular basis, especially if you have had unprotected sex and/or more than one sex partner.
Early stages of syphilis are easily cured with antibiotics. The most common treatment is penicillin or doxycycline once a week for three weeks in alternate buttocks. Other antibiotics, including tetracyclines and macrolides are used when there is penicillin allergy. Here’s some good news: these antibiotics respond promptly. Also, the treponeme shows no signs of developing resistance to penicillin or any other antibiotics.
Someone who has been infected for a while will need treatment for a longer period of time. Unfortunately, damage to the body from the late stage of syphilis cannot be treated. However, even in the late stage, it is important to get treatment. This can prevent further damage to the body. Anyone with whom you’ve had unprotected sex also should be checked for syphilis immediately.
Being treated for syphilis does not make you immune. You CAN catch it more than once.
The best way to prevent any STD is to not have sex. However, for people who decide to have sex, it’s important to use protection. Latex condoms are effective against most STDs; however, if there are any sores or rashes, avoid sex until the person has seen a doctor for treatment.
If you’ve read this far, here’s some fun facts on the origins of syphilis.
Where did syphilis come from?
In David Barlow’s book, Sexually Transmitted Infections (The Facts), he explains that there are a few views as to the origins of syphilis in Europe. Some blame Columbus (actually probably his crew) for bringing it to Barcelona from North America in 1493. The siege of Naples took place the following year when some infected Spaniards joined France. By the spring of 1495 a dreadful plague had broken out. The English called it the French disease. The French called it the Italian disease; the indecisive Italians called it the French and Spanish disease, while the Spanish called it the disease of Hispaniola. Neopolitan soldiers labeled it Mal Franzoso, the French disease, in 1495. Their French opponents called it “the Neapolitan disease.” The Russians dubbed it “the Polish sickness.” The Poles attributed it to Germany. The Japanese named the sores “Chinese ulcers.” And it was known for centuries as “the great” (as opposed to the “small”) pox.
Medieval cities banished syphilitics outside their gates or “cured” them with mercury ointments that made their bodies shake and teeth fall out before they died. The pre-Columbians school argues that it was around in Europe in pre-Christian day. There are many references in the Old Testament to conditions with signs and symptoms that could be syphilis. One translation, from Psalms, threatens ‘…the Lord shall smite you in the knees and in the legs with a sore botch that cannot be healed from sole of thy foot to the top of thy head.’
Pope Julius II, Henry VIII, Ivan the Terrible, George Washington and Nietzsche were all syphilitics.
- You CAN get syphilis from oral sex.
- This first phase is the most infectious stage characterized by a red, firm, painless and sometimes wet ulcer or open sore.
- The second phase occurs 3-8 weeks after infection and is characterized by a flu-like condition. This is also an infectious time.
- If you want to get a blood test for syphilis, ask your doctor for an RPR. That’s the code, so you can keep the results more hidden.
- African Americans are 34 times more likely to have syphilis than whites.
- Being treated for syphilis does not make you immune. You CAN catch it more than once.
- Article: KidsHealth.org – Syphilis
- Government Publication: Wisconsin Division of Public Health – Disease Fact Sheet
- Article: EverydayHealth.com – Syphilis Cases Climbing Among Gay Men
- Book: “Sexually Transmitted Infections” by David Barlow
DISCLAIMER: The information contained in this post is intended to inform readers and is not intended to replace specific advice from a health care professional.